This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
50 years Years old male came to OPD with cheif complaints of shortness of breath since 10 days.
Complaints of decreased urine output,nausea,B/L pedal edema and constipation since 10 days.
Patient was aparently asymptomatic 15 years back, then developed B/L pedal edema , shortness of breath and was brought to our hospital 1 session of HD done.Patient was diagnosed with CKD 15 years back and was treated conservatively(on and off).
Now again 10 days back he came to OPD.
Past History :-
K/C/O HTN since 10 months and on regular medications.
Not a known case of DM , asthama , TB , Thyroid , epilepsy.
Personal History :-
Diet : mixed
Apetite : decreased since 10 days.
Sleep : adequate.
Bowel movements : irregular
Decreased urine output.
No any addictions.
On examination, patient is C/C/C .
Pallor present.
B/L pitting edema present till knees.
No cyanosis , icterus, clubbing , lymphadenopathy.
Temperature - 98.5*F
PR - 112/ min
RR - 18cpm
BP - 110/90 mmhg
Spo2 - 99% at RA
Grbs - 115 mg%
CVS :- S1 , S2 heard
RS - BAE present
P/A - soft and non tender
CNS - No focal Neurological deficet.
RFT :-
Serum Albumin :-
USG :-
Serology:-
Serology :-
Serology:-
CBP:-
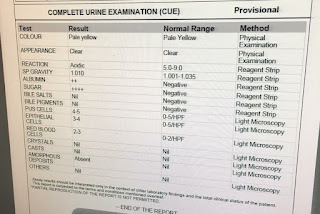
CUE:-
Provisional diagnosis :-
Chronic kidney disease with Polycystic kidney disease and K/C/O HTN since 10 months.
Updates
Day 2 :
Urea :- 219 mg/dl
Creatinine : 17.5 mg/dl
Hb : 5.2 gm%
1 session of HD was performed on 18th along with transfusion of 1 unit of PRBC.
S :-
B/L Pedal edema present.
Decreased urine output.
Nausea present.
O :-
BP - 160/80 mmhg
PR - 81 bpm
Temp - afebrile
RR -16cpm
Spo2 - 99% at RA
P :-
1) Fluid restriction less than 1L / day
2) Salt restriction less than 2.4 gm/day
3) TAB. LASIX 40MG PO/TID
4) TAB. NICARDIA 20 MG PO/BD
5) TAB OROFER-XT PO/OD
6) TAB NODOSIS 550MG PO/BD
7) TAB SHECAL 500MG PO/OD
8) INJ ERYTHROPOIETIN 4000IU S/C WEEKLY ONCE
9) INJ IRON SUCROSE 2 AMP IN 100ML NS IV DURING DIALYSIS
10) TAB ARKAMINE 0.1MG PO/OD
11) TAB ZOFER 4MG PO/TID
day 3:
Urea : 109 mg/dl
Creatinine : 11.3 mg/dl
Hb : 7.4 gm%
S :-
B/L Pedal edema present.
Decreased urine output.
Nausea present.
O :-
BP - 160/80 mmhg
PR - 81 bpm
Temp - afebrile
RR -16cpm
Spo2 - 99% at RA
P :-
1) Fluid restriction less than 1L / day
2) Salt restriction less than 2.4 gm/day
3) TAB. LASIX 40MG PO/TID
4) TAB. NICARDIA 20 MG PO/BD
5) TAB OROFER-XT PO/OD
6) TAB NODOSIS 550MG PO/BD
7) TAB SHECAL 500MG PO/OD
8) INJ ERYTHROPOIETIN 4000IU S/C WEEKLY ONCE
9) INJ IRON SUCROSE 2 AMP IN 100ML NS IV DURING DIALYSIS
10) TAB ARKAMINE 0.1MG PO/OD
11) TAB ZOFER 4MG PO/TID
Day 4:
Urea : 115 mg/dl
Creatinine : 11.2 mg/dl
Hb : 6.8 gm%
1 session of HD was done along with transfusion of 1 unit of PRBC.
S :-
B/L Pedal edema present.
Decreased urine output.
Nausea present.
O :-
BP - 160/80 mmhg
PR - 81 bpm
Temp - afebrile
RR -16cpm
Spo2 - 99% at RA
P :-
1) Fluid restriction less than 1L / day
2) Salt restriction less than 2.4 gm/day
3) TAB. LASIX 40MG PO/TID
4) TAB. NICARDIA 20 MG PO/BD
5) TAB OROFER-XT PO/OD
6) TAB NODOSIS 550MG PO/BD
7) TAB SHECAL 500MG PO/OD
8) INJ ERYTHROPOIETIN 4000IU S/C WEEKLY ONCE
9) INJ IRON SUCROSE 2 AMP IN 100ML NS IV DURING DIALYSIS
10) TAB ARKAMINE 0.1MG PO/OD
11) TAB ZOFER 4MG PO/TID
Day 5
Urea : 42 mg/dl
Creatinine : 4.9 mg/dl
Hb : 8.4 gm%
1 session of HD was done.
S :-
B/L Pedal edema present.
Decreased urine output.
O :-
BP - 150/80 mmhg
PR - 83 bpm
Temp - afebrile
RR -17cpm
Spo2 - 99% at RA
P :-
1) Fluid restriction less than 1L / day
2) Salt restriction less than 2.4 gm/day
3) TAB. LASIX 40MG PO/TID
4) TAB. NICARDIA 20 MG PO/BD
5) TAB OROFER-XT PO/OD
6) TAB NODOSIS 550MG PO/BD
7) TAB SHECAL 500MG PO/OD
8) INJ ERYTHROPOIETIN 4000IU S/C WEEKLY ONCE
9) INJ IRON SUCROSE 2 AMP IN 100ML NS IV DURING DIALYSIS
10) TAB ARKAMINE 0.1MG PO/OD
11) TAB ZOFER 4MG PO/TID
Day 6
Urea : 36 mg/dl
Creatinine : 2.9 mg/dl
Hb : 9.1 gm%
1 session of HD was done along with transfusion of 1 unit of PRBC.
S :-
B/L Pedal edema present.
Decreased urine output.
Nausea present.
O :-
BP - 130/80/90 mmhg
PR - 82 bpm
Temp - afebrile
RR -16cpm
Spo2 - 99% at RA
P :-
1) Fluid restriction less than 1L / day
2) Salt restriction less than 2.4 gm/day
3) TAB. LASIX 40MG PO/TID
4) TAB. NICARDIA 20 MG PO/BD
5) TAB OROFER-XT PO/OD
6) TAB NODOSIS 550MG PO/BD
7) TAB SHECAL 500MG PO/OD
8) INJ ERYTHROPOIETIN 4000IU S/C WEEKLY ONCE
9) INJ IRON SUCROSE 2 AMP IN 100ML NS IV DURING DIALYSIS
10) TAB ARKAMINE 0.1MG PO/OD
11) TAB ZOFER 4MG PO/TID
Day 7
Hb : 9.8%
S :-
B/L Pedal edema present.
Decreased urine output.
O :-
BP - 130/80 mmhg
PR - 81 bpm
Temp - afebrile
RR -17cpm
Spo2 - 99% at RA
P :-
1) Fluid restriction less than 1L / day
2) Salt restriction less than 2.4 gm/day
3) TAB. LASIX 40MG PO/TID
4) TAB. NICARDIA 20 MG PO/BD
5) TAB OROFER-XT PO/OD
6) TAB NODOSIS 550MG PO/BD
7) TAB SHECAL 500MG PO/OD
8) INJ ERYTHROPOIETIN 4000IU S/C WEEKLY ONCE
9) INJ IRON SUCROSE 2 AMP IN 100ML NS IV DURING DIALYSIS