This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
Chief complaints
>fever since 3 days
>headache since 2 days
History of presenting Illness
Patient was apparently asymptomatic 3 days ago then developed fever, high grade a/w chills, not associated with diurnal variation, relieving on medication
H/O headache present since 2 days in frontal region, continuous,
No H/O vomiting, loose stools
No H/O nausea, abdominal distension
No H/O rash, chough, cold
No H/O burning mituration, dysurea
Past H/O
Not a K/C/O DM, HTN, thyroid disease, BA
PERSONAL HISTORY :
DIET - MIXED
APPETITE -NORMAL ,
BOWEL MOVEMENT - REGULAR ,
BLADDER MOVEMENTS - REGULAR,
ALCOHOL ADDICTION, LAST BINGE 3 DAYS BACK 60 ML WHISKY
FAMILY HISTORY -
NAD
ON EXAMINATION -
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALOR, ICTRUS, CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA
VITALS -
TEMPERATURE - 99.1
PULSE RATE - 84 BPM
BLOOD PRESSURE - 110/70 MM OF HG
RESPIRATORY RATE - 16
SPO2 - 99 % AT ROOM AIR
SYSTEMIC EXAMINATION -
PER ABDOMEN : NON DISTENDED, SOFT NON-TENDER, NO GAURDING/RIGIDITY
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT ,NORMAL VESICULAR BREATH SOUNDS
CENTRAL NERVOUS SYSTEM : NAD
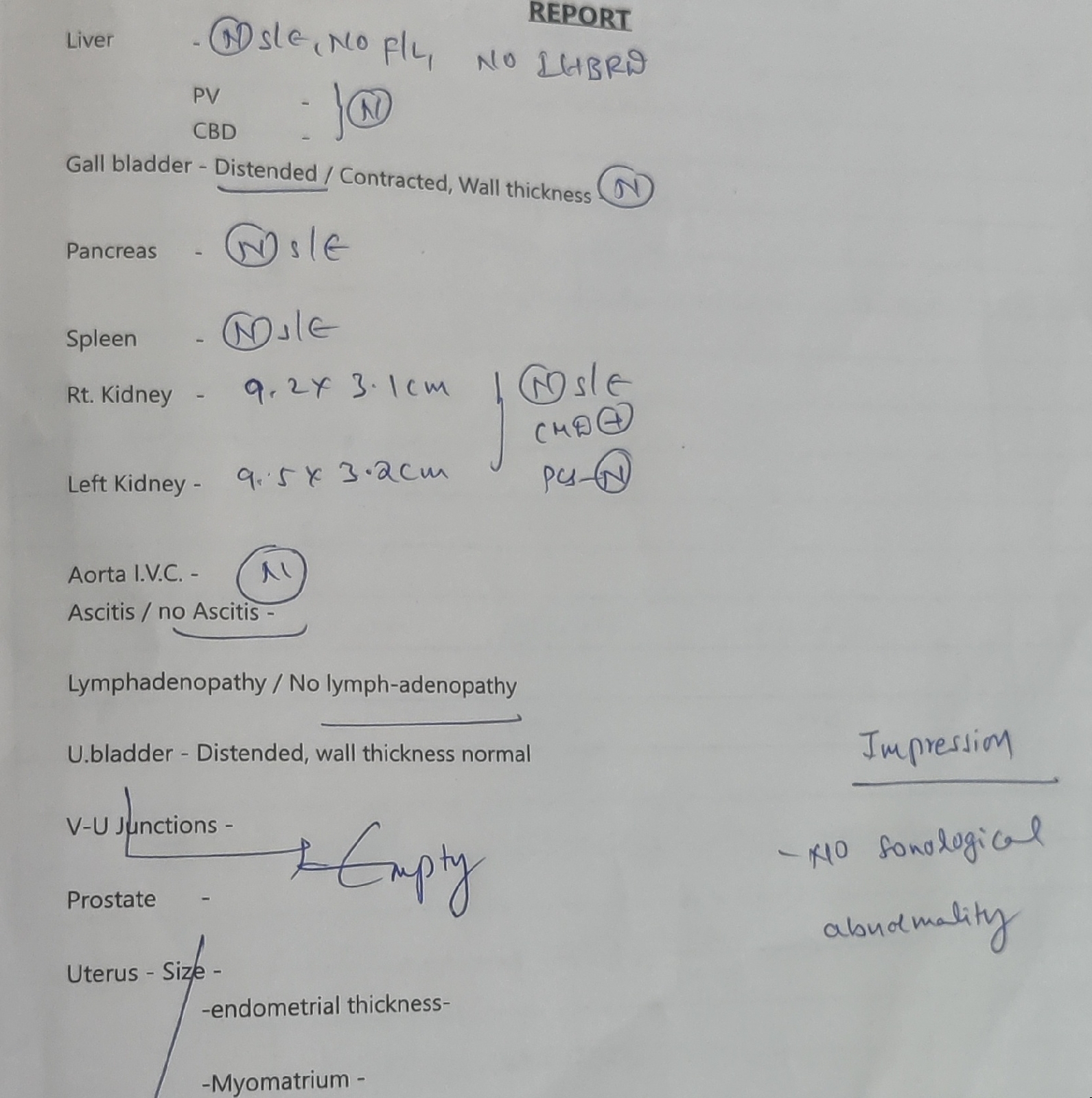
Investigations
ECG
Chest X-ray
CUE (2/3/22)
Albumin: +
Sugar: ++++
Pus cells: 4-5
Epithelial cells: 3-4
HEMOGRAM
HB 14.3
TC 2800
PLT 92000
MCV 80.2
PCV 41.2
MCH 27.5
MCH 34.3
SMEAR - NORMOCYTIC NORMOCHROMIC, WITH BICYTOPENIA
SMEAR FOR MALARIAL PARASITE - Negative
BGT - O +ve
CUE
ALB - trace
Sugar - nil
Puscells - 2-4
Epithelial cells - 2-4
HbSAg - negative
HCV - negative
HIV - negative
Dengue serology
NS1 - +ve
IgG - negative
IgM - negative
RFT
Urea- 22
Creatinine-0.9
UA-4.1
Calcium-9.2
Phosphorus-2.5
Sodium-136
Potassium-3.8
Chloride-102
LFT
TB-1.37
DB-0.47
AST-84
ALT-49
ALP-168
TP-56
ALB-3.31
Diagnosis
Viral pyrexia
Treatment
Inj. Paracetamol 1g IV Stat
IVF NS/RL at 75ml/hr
T. Paracetamol 650mg PO TID
Day 1
S-C/o headache, neck pain subsided, one fever spikes today
O-
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALOR, ICTRUS, CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA
VITALS -
TEMPERATURE - 98.1
PULSE RATE - 75 BPM
BLOOD PRESSURE - 120/80 MM OF HG
RESPIRATORY RATE - 17
SPO2 - 100 % AT ROOM AIR
SYSTEMIC EXAMINATION -
PER ABDOMEN : NON DISTENDED, SOFT NON-TENDER, NO GAURDING/RIGIDITY
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT ,NORMAL VESICULAR BREATH SOUNDS
CENTRAL NERVOUS SYSTEM : NAD
HEMOGRAM
HB 16
TLC 3000
PCV 46.6
MCV 82.9
MCH 28.9
MCHC 34.2
Plt 90,000
P. S normocytic, normochromic with bicytopenia
A-
viral pyrexia with thrombocytopenia with NS1POSITIVE
P-
Inj. Optineuron in 100ml NS over 30 mins
IVF NS/RL at 150ml/hr
T. Paracetamol 650mg PO TID
S-C/o headache,neck pain subsided, no fever spikes today
O-
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALOR, ICTRUS, CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA, no petichiae
VITALS -
TEMPERATURE - 98.3
PULSE RATE - 82 BPM
BLOOD PRESSURE -
110/70 MM OF HG supine
110/70 mmHg standing
RESPIRATORY RATE - 19
SPO2 - 99 % AT ROOM AIR
SYSTEMIC EXAMINATION -
PER ABDOMEN : NON DISTENDED, SOFT NON-TENDER, NO GAURDING/RIGIDITY
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT ,NORMAL VESICULAR BREATH SOUNDS
CENTRAL NERVOUS SYSTEM : NAD
HEMOGRAM
HB 15.9
TLC 2300
PCV 46.3
MCV 82.9
Plt 50,000
P. S NORMOCYTIC NORMOCHROMIC WITH neutropenia and thrombocytopenia
A-
viral pyrexia with thrombocytopenia with NS1POSITIVE
P-
Inj. Optineuron in 100ml NS over 30 mins
IVF NS/RL at 150ml/hr
T. Paracetamol 650mg PO TID
S-C/o headache,neck pain subsided, no fever spikes today
O-
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALOR, ICTRUS, CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA, no petichiae
VITALS -
TEMPERATURE - 96.9
PULSE RATE - 85 BPM
BLOOD PRESSURE -
110/70 MM OF HG supine
110/70 mmHg standing
RESPIRATORY RATE - 19
SPO2 - 98 % AT ROOM AIR
SYSTEMIC EXAMINATION -
PER ABDOMEN : NON DISTENDED, SOFT NON-TENDER, NO GAURDING/RIGIDITY
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT ,NORMAL VESICULAR BREATH SOUNDS
CENTRAL NERVOUS SYSTEM : NAD
HEMOGRAM
HB 15.1
TLC 2900
PCV 45.2
MCV 80.9
Plt 41,000
P. S NORMOCYTIC NORMOCHROMIC WITH neutropenia and thrombocytopenia
Platlet count
Day 1 - 92,000
Day 2 - 90,000
Day 3 - 50,000
Day 4 - 41,000
A-
viral pyrexia with thrombocytopenia with NS1POSITIVE
P-
Inj. Optineuron in 100ml NS over 30 mins
IVF NS/RL at 150ml/hr
T. Paracetamol 650mg PO TID